Learn to recognize the subtle and overt signs of childhood anxiety with this in-depth guide covering developmental stages, physiological symptoms, and when to seek professional help.
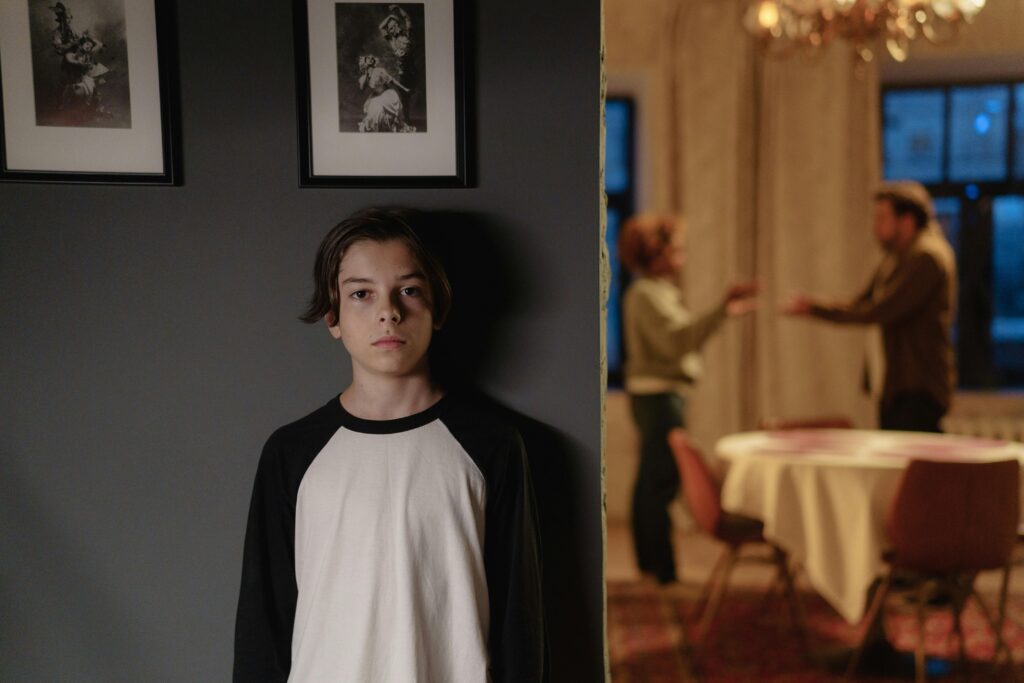
Introduction: The Hidden Epidemic of Childhood Anxiety
Anxiety disorders now affect 1 in 5 children, yet symptoms frequently go unrecognized because they manifest differently than in adults. Unlike temporary worries, childhood anxiety persists for weeks or months, interfering with development, learning, and social connections. This expanded guide helps parents distinguish normal developmental fears from clinically significant anxiety across all age groups.
Section 1: Developmental Variations in Anxiety Expression
Preschoolers (Ages 3-5)
- Physical Symptoms Dominant:
- Unexplained stomachaches/headaches
- Excessive clinginess (won’t separate at daycare)
- Regression in toilet training
- Sleep disturbances: Night terrors, refusal to sleep alone
- Behavioral Signs:
- Extreme distress over small routine changes
- Repetitive reassurance-seeking (“Are you sure?”)
- Avoidance of noisy/public places
Case Example: 4-year-old Liam screams when parents leave the room, despite previously enjoying independence.
Elementary School (Ages 6-11)
- Cognitive Signs Emerge:
- Perfectionism leading to erased homework
- Catastrophic thinking (“What if the dog dies?”)
- Time-consuming rituals (checking, counting)
- Social Impacts:
- Frequent nurse visits to avoid class
- Decline in academic performance
- Over-apologizing for minor mistakes
Case Example: 8-year-old Sofia redoes her handwriting 10 times until “it feels right.”
Teens (Ages 12-18)
- Internalized Symptoms:
- Excessive self-criticism
- Social withdrawal despite FOMO
- Substance experimentation to self-medicate
- Physical Manifestations:
- Panic attacks mistaken for asthma
- Hair pulling/skin picking
- Unexplained vomiting before school
Case Example: 14-year-old Raj skips lunch daily, claiming he’s “not hungry” (but actually nauseous from anxiety).

Section 2: The 7 Most Overlooked Anxiety Signs
1. “Clumsiness” and Coordination Issues
- Anxiety disrupts proprioception (body awareness)
- Tripping, spilling, or knocking things over increases
- Differentiate from: True motor skill disorders
2. Voice Changes
- Sudden baby talk regression
- Monotone/flat affect when stressed
- Throat clearing (vocal tic from tension)
3. Time Disorientation
- Losing track of conversations
- Chronic lateness despite effort
- Mechanism: Prefrontal cortex overload
4. Sensory Seeking/Avoidance
- Chewing shirt collars/pencils
- Refusing certain clothing textures
- Covering ears at normal sounds
5. “Imaginary” Illnesses
- Reporting phantom pains that move locations
- Mimicking others’ symptoms
- Key clue: Symptoms vanish during preferred activities
6. Over-Responsibility
- Parenting siblings excessively
- Anxiety about adult problems (bills, health)
- Risk factor: Parentification trauma
7. Humor as Camouflage
- Deflecting with jokes when uncomfortable
- Laughing at inappropriate times
- Masking strategy: Especially common in gifted kids

Section 3: Anxiety vs. Other Conditions
Anxiety vs. ADHD
| Trait | Anxiety | ADHD |
|---|---|---|
| Focus Issues | Fear of mistakes | Easily distracted |
| Fidgeting | Tense movements | Energy release |
| Impulsivity | Rare | Common |
Anxiety vs. Autism
| Trait | Anxiety | Autism |
|---|---|---|
| Social Challenges | Fear-driven | Skill-deficit |
| Routines | For comfort | For predictability |
| Eye Contact | Avoids when anxious | Consistently atypical |
Section 4: Physiological Red Flags
1. Sleep Architecture Changes
- Increased sleep latency (hours to fall asleep)
- Early morning waking (4-5 AM)
- Increased REM density (vivid stressful dreams)
2. Appetite/Growth Patterns
- Chewing without swallowing
- Picky eating worsening
- Growth curve dips (stress hormones affect IGF-1)
3. Immune System Impacts
- Frequent strep/ear infections
- Eczema flare-ups
- Allergy symptom exacerbation
Section 5: When to Seek Professional Help
Urgent Intervention Needed If:
- Self-harm behaviors emerge
- School refusal lasts >2 weeks
- Weight loss exceeds 5% body weight
Specialized Evaluations
- Psychoeducational testing (for learning anxiety)
- Play therapy assessment (ages 3-7)
- Biofeedback (for physical symptoms)
Treatment Options
| Approach | Best For | Course Length |
|---|---|---|
| CBT | Ages 6+ | 12-20 sessions |
| PCIT | Ages 2-7 | 14 weeks |
| SSRIs | Severe cases | 6-12 months |
Section 6: Parental Support Strategies
1. The 5-Second Rule
Pause before reassuring to avoid reinforcing anxiety cycles. Instead of “You’re safe,” try:
- “I see this feels scary. What do you need?”
2. Sensory Toolkits
- For younger kids: Fidget bracelets, chewy necklaces
- For teens: Acupressure rings, weighted lap pads
3. Worry Time Scheduling
- Daily 15-minute “worry session”
- Use timer to contain rumination
- Journal or draw concerns
Section 7: School Accommodations
Formal 504 Plan Options
- Testing in small groups
- Unlimited bathroom passes
- Alternative lunch arrangements
Teacher Collaboration Tips
- Secret signals for breaks
- Advance notice for schedule changes
- “Safe seat” near exit
8 FAQs About Childhood Anxiety
1. Can toddlers have anxiety disorders?
Yes—as young as 18 months. Look for:
- Excessive stranger danger
- Sleep refusal beyond typical phases
2. Do anxious kids outgrow it?
Without treatment, 60% develop chronic anxiety. Early intervention changes trajectories.
3. Should I force my child to face fears?
Gradual exposure works, but never flood. Try the “ladder approach” with small steps.
4. Are meltdowns a sign of anxiety?
In overcontrolled kids, yes—outbursts often follow prolonged internal stress.
5. Can food affect childhood anxiety?
Emerging research links:
- Food dyes to hyperactivity
- Blood sugar swings to panic-like symptoms
6. How do I find the right therapist?
Look for:
- Play therapy certification (under age 10)
- SPACE program training (parent-focused treatment)
7. When should medication be considered?
For:
- Suicidal ideation
- School refusal >1 month
- Weight loss from anxiety
8. Can schools diagnose anxiety?
No—but they can recommend evaluations. Always seek clinical psychologist assessment.
Final Thoughts: Early Intervention Matters
Childhood anxiety left unaddressed predicts:
✅ 3x higher risk of adolescent depression
✅ Impaired social skill development
✅ Academic underachievement
📌 Call to Action: If you notice 3+ signs persisting over 6 weeks, consult a child psychologist—not just your pediatrician.










